Categories
Most Popular
Dahi Baray Recipe
Search This Blog
- January 20261
- December 20254
- November 20254
- October 20257
- September 20256
- August 20257
- July 20257
- June 20252
- May 20258
- April 20255
- March 20252
- February 20256
- January 20256
- December 20245
- November 20245
- October 20248
- September 20245
- August 20247
- July 20245
- June 20243
- May 20249
- April 20244
- March 20248
- February 20246
- January 202412
- December 20238
- November 20239
- October 202312
- September 202310
- August 202310
- July 20236
- June 20237
- May 202310
- April 20239
- March 20235
- February 20233
- January 20238
- December 20225
- November 20229
- October 202212
- September 20227
- August 202211
- July 20224
- June 202210
- May 20228
- April 20221
- March 202224
- February 202214
- January 202216
- December 202112
- November 202116
- October 202117
- September 20219
- August 202122
- July 202117
- June 202128
- May 20211
- April 20213
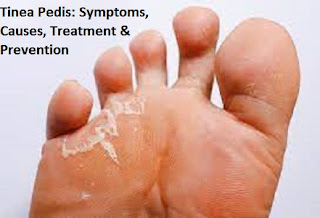
Tinea Pedis: Symptoms, Causes, Treatment & Prevention
A fungal infection that is very contagious and affects the skin on the feet is known as athlete's foot (tinea pedis).
Although not serious, an athlete's foot can occasionally be difficult to treat. You should contact your doctor as soon as possible if you think you may develop an athlete's foot and you have diabetes or a weak immune system.
Fungal skin infection known as athlete's foot (tinea pedis) usually begins in the space between the toes. It usually happens to persons whose shoes are too tight and their feet have become quite sweaty.
An itchiness and scaling of the skin are indications of athlete's foot. It is possible for the illness to spread through contaminated flooring, towels, or clothing.
Jockey itch and ringworm are two more fungal illnesses that are closely linked to athlete's foot. Antifungal medications can be used to treat it, but the illness frequently returns.
Also Read: Tinea Corporis (Body Ringworm): Symptoms, Causes, Diagnose, Treatment & Prevention
What is tinea pedis?
A dermatophyte fungal infection of the foot is known as tinea pedis. This is the most typical dermatophyte infection and is particularly common in hot, tropical cities.The most common involvement is in the interdigital; athlete's foot, a term used to refer to any form of tinea pedis, is another name for this type of disorder.
Symptoms:
One or both feet may be impacted by the athlete's foot. Typical indications and manifestations include:- Between the toes, scaly, peeling, or cracked skin.
- Itchiness, particularly immediately after removing socks and shoes.
- Inflamed skin that, depending on your skin tone, may look crimson, purple, or gray.
- Stinging or burning.
- Blisters.
- The skin on the bottom of the foot that rises the side is dry and scaly.
Causes:
The same kind of fungi (dermatophytes) that cause jock itch and ringworm can cause athlete's foot. The organisms develop best in warm, humid environments with damp shoes and socks.Factors at risk:
Athlete's foot is more likely to occur if you:- Wear closed-toe shoes often
- Sweat heavily
- Mats, carpets, bedding, clothing, and shoes should not be shared with someone who has a fungal infection.
- Go barefoot in public areas like locker rooms, saunas, swimming pools, and shared bathrooms and showers where the infection can spread.
Complications:
It is possible for the athlete's foot infection to spread to other warm, moist body areas. Many times, the same fungus that causes athlete's foot also causes jock itch. Because the fungus can spread through hands and towels, it is normal for the illness to move from the feet to the groin.Bacterial infections can sometimes result from athlete's foot.
How do you treat an athlete's foot?
Topical antifungal drugs available over-the-counter (OTC) are frequently effective in treating athlete's feet. Your doctor may recommend topical or oral prescription-strength antifungal medications if alternative treatments are ineffective in treating your infection. To help get rid of the illness, your doctor might also suggest certain at-home treatments.Prescription medications:
Your doctor may recommend the following prescription drugs to treat athlete's foot:Topical steroid medications to reduce painful inflammation oral antibiotics if bacterial infections develop due to raw skin and blisters topical, prescription-strength clotrimazole or miconazole oral antifungal medications such as itraconazole (Sporanox), fluconazole (Diflucan), or prescription-strength terbinafine (Lamisil)
Prevention:
You can prevent athlete's foot or stop others from getting it by following these tips:- Give your feet some room to breathe. Wear sandals whenever you can to maximize the amount of airflow on your feet.
- When you're at home, go barefoot to give your feet a break.
- Every day, wash your feet. Rinse and completely dry your feet, paying careful attention to the spaces between your toes, using warm, soapy water. If you are prone to athlete's foot, apply a medicinal powder for your feet (such as Tinactin, Gold Bond, or others) or another medicated powder such as Zeasorb.
- Often change your socks. If your feet get sweaty, change your socks more frequently than once a day. Socks that wick away moisture, like cotton ones, keep your feet drier than socks made of nylon.When you're in public, keep your feet safe. When near public swimming pools, showers, and locker rooms, wear water-resistant shoes or sandals.
- Recognize the factors that could lead to the conditions spreading. Don't share shoes or dirty towels and beds if you live together.
- Bell-Syer EM, et al. Oral treatments for fungal infections of the skin of the foot. Cochrane Database of Systematic Reviews. 2015; doi.10.1002/14651858.CD003584.pub2.
- Aaron DM. (2016). Athlete’s foot (tinea pedis).https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0024878/
- Crawford F, et al. Topical treatments for fungal infections of the skin and nails of the foot. Cochrane Database of Systematic Reviews. 2016; doi.10.1002/14651858.CD001434.pub2.
- Mayo Clinic Staff. (2018). Athlete’s foot. https://www.mayoclinic.org/diseases-conditions/athletes-foot/symptoms-causes/syc-20353841
- Satchell AC, et al. (2002). Treatment ofinterdigital tinea pedis with 25% and 50% tea tree oil solution: A randomized,placebo-controlled, blinded study. DOI: https://doi.org/10.1046/j.1440-0960.2002.00590.x
- Newman CC, et al. Clinical pearls in dermatology 2017. Disease-a-Month 2017; doi.org/10.1016/j.disamonth.2017.03.003.

0 Comments